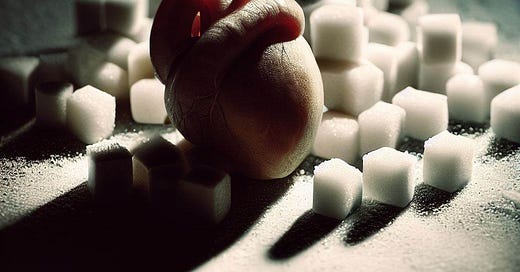
Do Statins Cause Diabetes?
The answer to this often highly contentious issue is, as always, it depends.
Life would be so much easier if there were binary, yes and no answers to every question that was important to us.
But there isn’t.
And even for so many of the questions you ‘think’ that have clear-cut answers, there actually aren’t.
You just think there are.
Let me explain.
Does speeding cause car crashes?
Most of you would agree that the answer here is …
Keep reading with a 7-day free trial
Subscribe to Dr Paddy Barrett to keep reading this post and get 7 days of free access to the full post archives.