When we say heart disease, what we typically mean is coronary atherosclerosis.
Atherosclerosis is, by definition, the retention of a cholesterol particle in the artery wall.
Every step of that process, from transition across the wall, particle retention, and subsequent metabolic processes that accelerate plaque development and the factors that cause it to rupture, are all connected to inflammation1.
Inflammation, therefore, plays a crucial role in every step of the process, from plaque initiation to plaque rupture and heart attack.
Inflammatory conditions ranging from rheumatoid arthritis, gout or even acute viral infections have long been recognised as risk factors that increase the risk of cardiovascular disease23.
Reducing inflammation then becomes a key factor in reducing the risk associated with cardiovascular disease.
Measuring Inflammation
Multiple markers of inflammation can be measured, including4:
High Sensitivity CRP (hs-CRP)
Interleukin 1 Alpha & Beta
Interleukin 6
Interleukin 12
Interleukin 15 etc.
High-sensitivity CRP is the only one of these markers routinely evaluated in clinical practice.
The family of interleukins mentioned are usually reserved for research purposes but have been researched extensively.
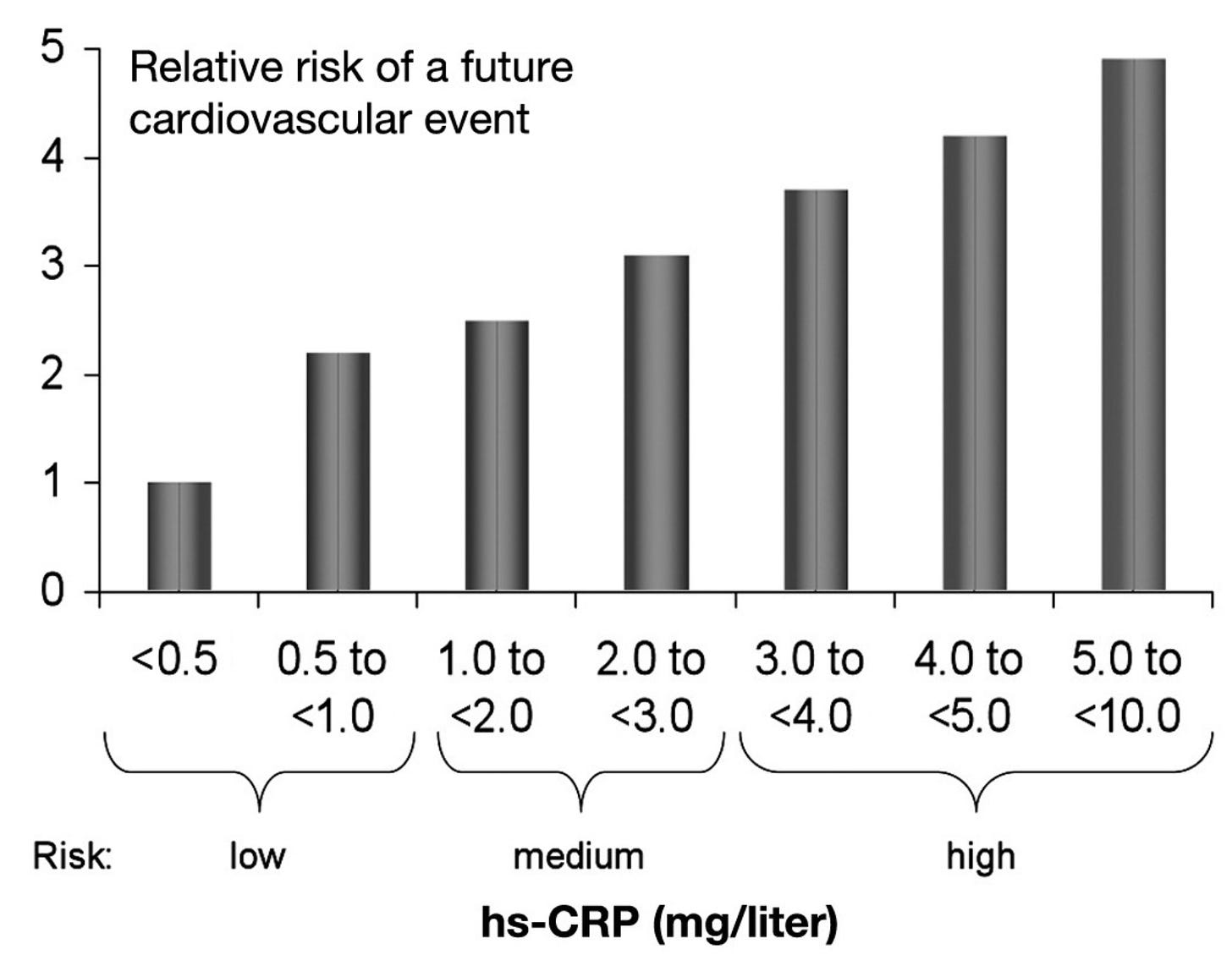
There is a linear increase in cardiovascular risk as levels of hsCRP increase5.
It is important to note that hs-CRP can be elevated for several reasons secondary to an underlying inflammatory process ranging from a chest infection to ongoing low-grade inflammation.
Strategies to Reduce Inflammation
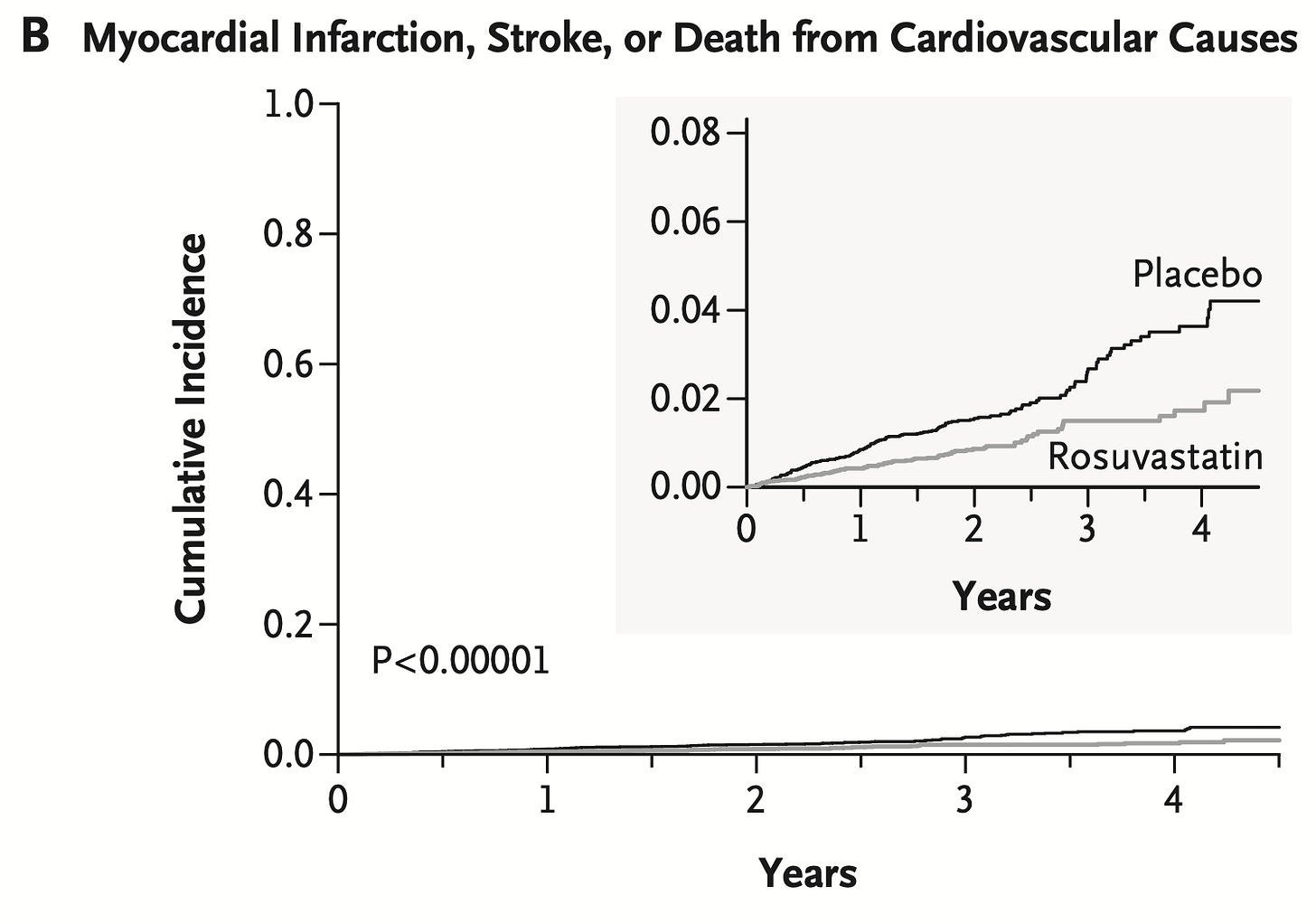
In those with relatively normal cholesterol levels but an elevated hs-CRP (>2mg/L ) and who were treated with statin therapy showed significantly fewer major cardiovascular events over a 2-year time frame6.
Not only were those who achieved a lower hs-CRP on statin therapy 47% less likely to have a heart attack or stroke the data also suggested they were less likely to die from any cause.
In such a relatively healthy cohort with normal-ish cholesterol levels, showing this over such a short period is rather impressive.
The big question that remained after this trial was whether the reduction in cardiovascular events was solely down to the cholesterol-lowering effect of statin therapy or whether it was also related to the reduction in levels of inflammation.
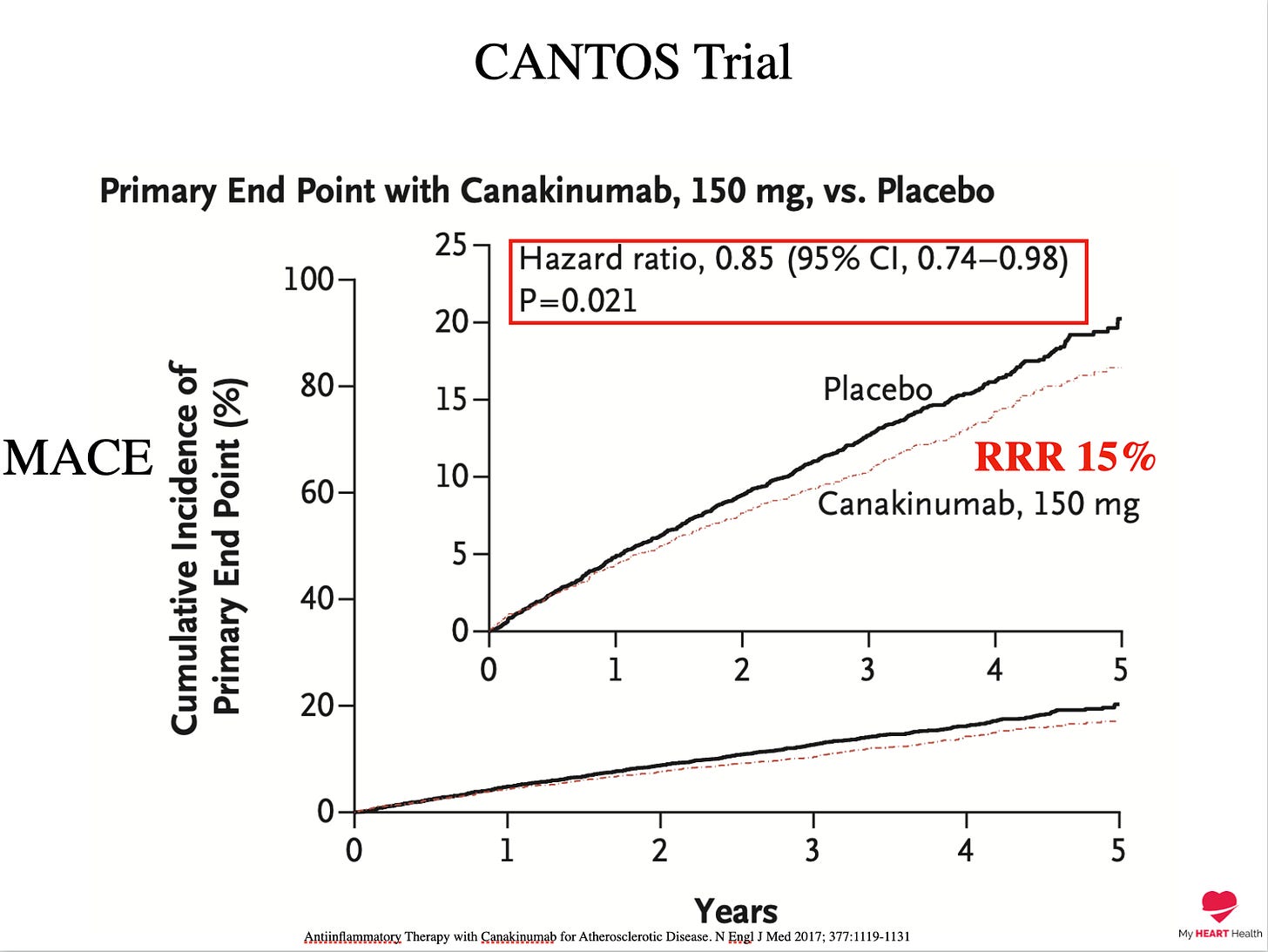
To answer this question, the CANTOS trial investigated whether lowering hsCRP alone with a selective interleukin 1 beta therapy called canakinumab would reduce cardiovascular events without lowering cholesterol levels7.
After almost four years, those with lower hs-CRP levels had 15% fewer cardiovascular events.
It seemed that lowering levels of inflammation by any means was now a new strategy for reducing cardiovascular events.
Until it wasn’t.
Several associational studies have shown fewer cardiovascular events in those on the anti-inflammatory medication methotrexate in those with rheumatoid arthritis.
However, when tested in a randomised control trial in those with prior heart attacks, no benefit was seen8.
We have continued to encounter conflicting results with anti-inflammatory therapies, including reductions in cardiovascular events with the use of colchicine, but with limited evidence that it reduces levels of hsCRP910.
Specific Pathways Matter
We are learning that inflammation plays a significant role in the development and acceleration of cardiovascular disease.
However, our therapies to reduce inflammation must be selectively targeted to achieve the most effect.
Immune modulation is challenging, and precision is required.
What about Non-Drug Therapies
The benefits of exercise have been established, and one of the mechanisms of this benefit may be reductions in inflammation as measured by the marker hsCRP.
Multiple studies have demonstrated reductions in hs-CRP, which may be why exercise is a cornerstone in preventing heart disease and why it is associated with longevity11.
Various supplements, including curcumin and fish oils, have demonstrated reductions in CRP1213. However, it is important to note that these compounds have not been tested to reduce cardiovascular events.
The COVID question
The relationship between COVID and anything COVID related to ANYTHING and EVERYTHING is complex and fraught with polarised opinions.
I make a conscious effort to avoid these debates for very good reasons.
But I will say this.
We have known for a VERY LONG time that viral infections can result in more inflammation and that higher levels of inflammation can result in more cardiovascular events1415.
Why would COVID be any different?
What We Know
Inflammation is a key driver of coronary artery disease.
Reducing inflammation is a vital part of reducing cardiovascular risk.
How we lower inflammation is complex and comes with differing levels of benefit.
Undoubtedly, anti-inflammatory therapies will form a cornerstone of our approach to cardiovascular disease in the future.
We just haven’t got all the details figured out just yet.
But we will get there.
The Role of Inflammation in Cardiovascular Disease. International Journal of Molecular Sciences. 2022; 23(21):12906.
Cardiovascular risk in inflammatory arthritis: rheumatoid arthritis and gout. Lancet Rheumatol. 2021 Jan;3(1):e58-e70.
Viruses and cardiovascular disease: from bad to worse. Nat Cardiovasc Res 1, 601–602 (2022).
The Role of Inflammation in Cardiovascular Disease. International Journal of Molecular Sciences. 2022; 23(21):12906.
High-sensitivity C-reactive protein predicts cardiovascular risk in diabetic and nondiabetic patients: effects of insulin-sensitizing treatment with pioglitazone. J Diabetes Sci Technol. 2010 May 1;4(3):706-16.
Rosuvastatin to Prevent Vascular Events in Men and Women with Elevated C-Reactive Protein. N Engl J Med 2008; 359:2195-2207
Antiinflammatory Therapy with Canakinumab for Atherosclerotic Disease. N Engl J Med 2017; 377:1119-1131
CIRT Investigators. Low-Dose Methotrexate for the Prevention of Atherosclerotic Events. N Engl J Med. 2019 Feb 21;380(8):752-762.
Colchicine in Patients with Chronic Coronary Disease. DOI: 10.1056/NEJMoa2021372
The Low Dose Colchicine after Myocardial Infarction (LoDoCo-MI) study: A pilot randomized placebo controlled trial of colchicine following acute myocardial infarction. Am Heart J. 2019 Sep;215:62-69.
Effects of exercise on c-reactive protein in healthy patients and in patients with heart disease: A meta-analysis. Heart Lung. 2016 May-Jun;45(3):273-82.
Effect of curcumin on C-reactive protein as a biomarker of systemic inflammation: An updated meta-analysis of randomized controlled trials. Phytother Res. 2022 Jan;36(1):85-97.
Fish oil supplementation lowers C-reactive protein levels independent of triglyceride reduction in patients with end-stage renal disease. Nutr Clin Pract. 2009 Aug-Sep;24(4):508-12.
Collins, S. D. Public Health Rep. 47, 2159 (1932).
Influenza vaccine as a coronary intervention for prevention of myocardial infarction
Heart 2016;102:1953-1956.





Great read, doc. Here's hoping my regular supplementation with Curcumin and Omega 3 combined with daily walking will hold off the statins at least for a few more years 😂
Very insightful! Thanks.