Miracle Weight Loss Medications. Real or Fools Gold?
Is A Medication For Durable Weight Loss Finally Here?
Munitions workers during World War 1 were often exposed to a chemical substance called DNP or 2,4-dinitrophenol.
This resulted in substantial weight loss as a result of an acceleration of their metabolism1.
As you might expect, this highly desired side effect resulted in DNP being sold as a ‘Miracle Weight Loss Pill’.
That it surely was.
There was just one catch.
It was killing people. Lots of them.
Since DNP, the world of weight loss medications has been a graveyard of failures.
There have been some successes, but most were modest and had many side effects.
Until now.
Enter GLP1 & GIP agonists.
You might know them as Wegovy (Semaglutide), Mounjaro (Terzepatide) or ‘those injections that everyone is on at the moment to magically lose weight’.
These classes of medications have been used for quite some time in patients with diabetes but recently have been tested in those without diabetes but who have obesity.
The results are nothing short of amazing.
As doctors, we are constantly being sold on the next ‘miracle treatment’, but rarely does it ever pan out.
This time might be different.
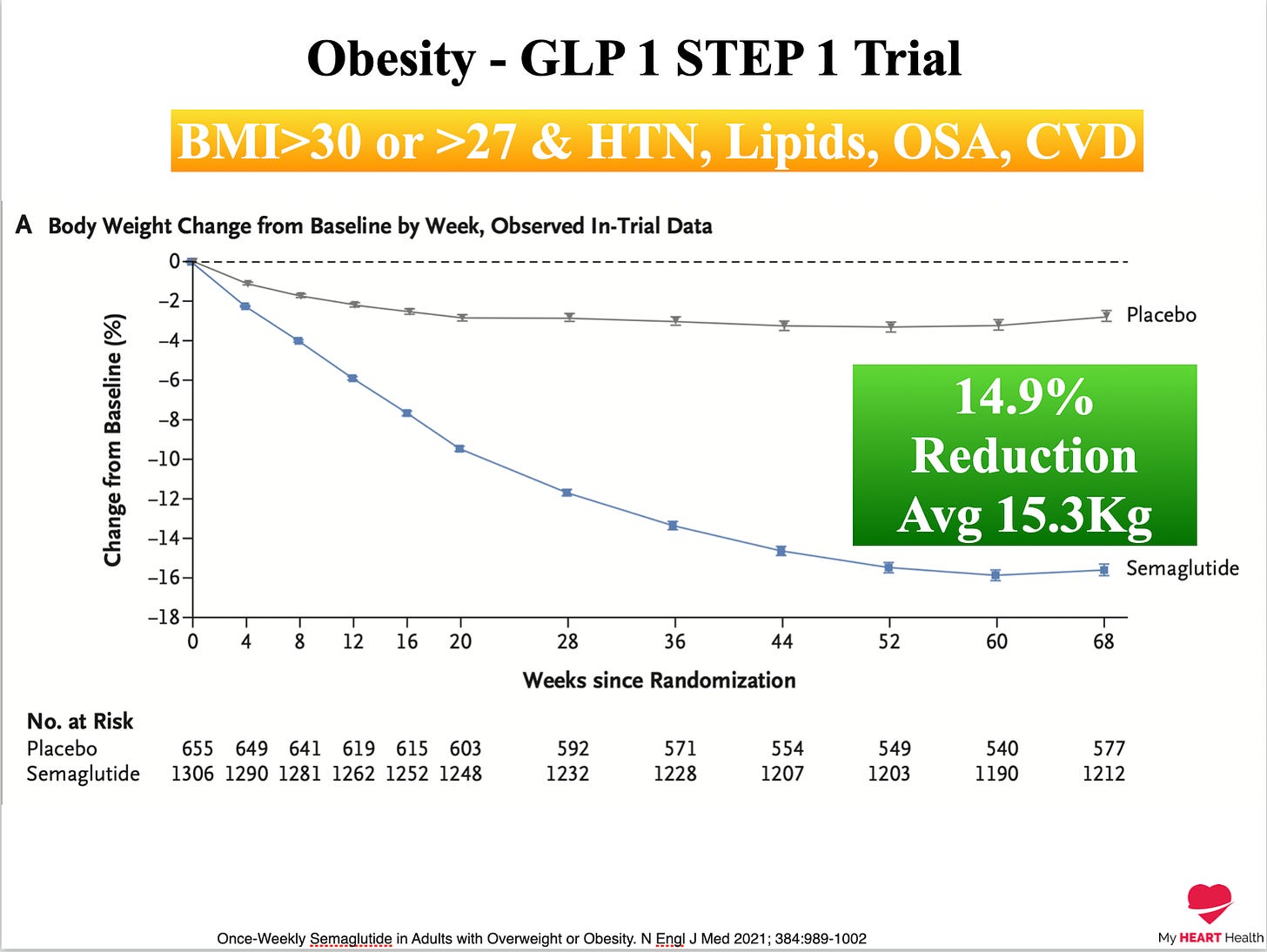
In those with obesity and an average starting weight of 107kg, patients treated with semaglutide lost, on average, 15% of their body weight or approximately 15 kg in just over one year2.
53% of patients lost more than 15% of their body weight, and 37% lost more than 20% of their body weight.
Put simply, we have seen nothing like this before in the world of weight loss, with the exception of bariatric surgery.
In those treated with tirzepatide, a combination GLP1 and GIP agonists, the results were even more impressive.
Patients treated at the higher dose of 15mg had, on average, a 20% loss in body weight, accounting for more than 57% of patients in that group3.
In addition to weight loss, a host of other cardiometabolic parameters also improved including4:
Liver function tests - Likely less fatty liver
Better blood pressure
Lower triglycerides
How do they work?
Both therapies primarily act on hormone regulation of the gut resulting in both delayed stomach emptying, which increases the sense of satiety and also by decreasing hunger signals in the brain5.
The net effect is a reduction in caloric intake.
The exact mechanisms as to how they work are still debated, but the bottom line is they work.
The next obvious question becomes:
Will I need these medications for life?
To answer that question, we need to look at two recent studies evaluating what happens when these medications are stopped and when they are continued.
As you can see from the graph below, when semaglutide was stopped at the end of the trial, a significant amount of patients regained much of the weight they had previously lost6.
Not all of it. But a lot.
For those who continued on the medication, the outcomes were very different.
Maintaining the therapy resulted in persistent weight loss and little to no weight gain over extended periods.
These two points have led many to comment that these drugs are not sustainable solutions to the problem of obesity7.
This pushback, I think, is entirely reasonable, but you have to ask what problem you are trying to address; an individual one or a societal one.
For individuals, these medications are absolute life changers.
As a solution to the population-level issue of obesity, they are not a good solution.
That will require enormous environmental and societal change.
But for people struggling with obesity today, waiting on this latter point is not really an option.
Additionally, when we start patients on cholesterol-lowering or blood pressure-lowering medications, they are usually for the long term.
Why would these classes of medications be any different?
Not All Upside
Although these therapies are a huge step forward in the treatment of obesity, they also come with downsides.
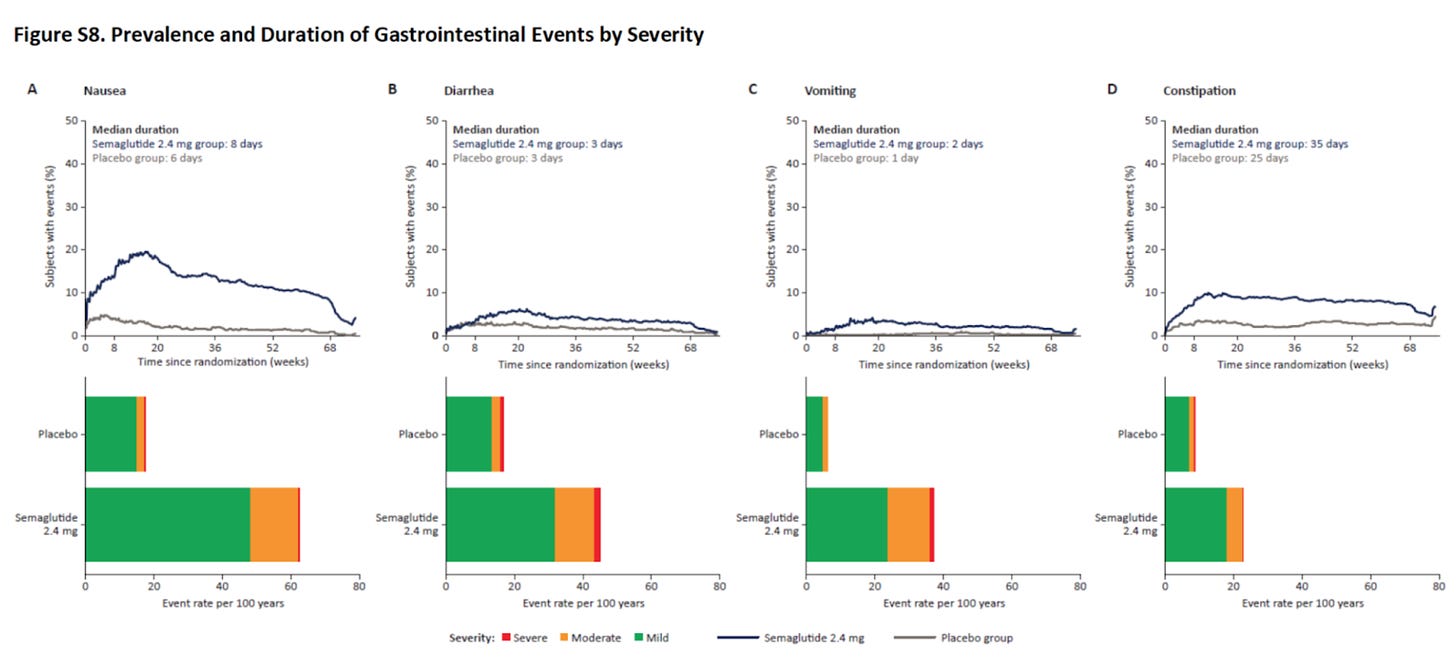
Many patients struggle with nausea, particularly in the initial phase of the therapy.
Some just cannot tolerate the treatment, even at the lowest doses8.
The other massive barrier is cost.
Most insurers or governments do not cover medical treatments for obesity, and this means that patients typically pay for these medications out of pocket.
These out-of-pocket expenses vary greatly depending on which country you are in.
For those in the United States, that figure can be anywhere up to $30,000 per year. For those in Europe, that figure can be in the range of about €2,000 per year.
Yes. It probably makes sense for someone in the US to fly to another country to get it if they need to.
Madness.
Additionally, there is also a huge black market for these treatments, and pharmacies are routinely out of stock.
Where Do I See Their Use?
These treatments are a massive step forward for many patients. But what needs to be taken into account is that these medications result in weight loss alone.
They do not improve muscle mass or increase V02 Max, which are fitness metrics highly correlated with improved health metrics.
But this just means that patients need to both continue or increase their exercise regime in addition to the weight loss they experience on these treatments.
Additionally, not all patients need full doses of these therapies. Many patients get to their target weight with only half the usual dose.
Just like blood pressure medications, we don’t need to use the full strength if we have already gotten to target.
These therapies are incredibly effective treatments for those with obesity, but losing 15% of your body weight when you are well over 100 kg still leaves you likely well above your ideal visceral fat mass target.
Lastly, these are treatments, not prevention tools, for obesity.
We, of course, need to modify our environments so that we are not massively incentivised into the behaviours that result in obesity, but that process may take years or never happen.
For the huge percentage of those struggling with obesity, these therapies are a lifeline.
They are tools.
Not a panacea.
We should view them as such.
https://theconversation.com/weight-loss-drug-made-from-war-chemicals-gets-deadly-new-reach-online-40647
Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med 2021; 384:989-1002
Tirzepatide Once Weekly for the Treatment of Obesity. NEJM June 4, 2022
Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med 2021; 384:989-1002
Effects of GLP-1 on appetite and weight. Rev Endocr Metab Disord. 2014 Sep;15(3):181-7.
Weight regain and cardiometabolic effects after withdrawal of semaglutide: The STEP 1 trial extension. Diabetes Obes Metab. 2022; 24( 8): 1553- 1564.
Two-year effect of semaglutide 2.4 mg on control of eating in adults with overweight/obesity: STEP 5. Obesity (Silver Spring). 2023 Jan 18.
Once-Weekly Semaglutide in Adults with Overweight or Obesity. N Engl J Med 2021; 384:989-1002







Interesting, I didn't know these meds worked on the satiety end of the process. That graph sure shoots up quick after treatment is ended. Also interesting to see that people lost a little bit of weight on the placebo.
My sister in law recently started on this medication. We are hoping it will save her life. Bariatric surgery didn't work for her. She is around 180 kg with all sorts of issues due to her weight. This might be her last hope.